Hans Huitink
@airwaymxacademy.bsky.social
Anesthesiologist🇳🇱Founder Airway Management Academy non-profit airway teaching #AAF25 | Mobile Critical Care Support😷🚑🩺 | AirAmbulance🛩 @AirwayTriageApp
created November 20, 2024
756 followers 1,135 following 116 posts
view profile on Bluesky Posts
 Stu Marshall (@hypoxicchicken.medsky.social) reposted reply parent
Stu Marshall (@hypoxicchicken.medsky.social) reposted reply parent
We had an MH susceptible pt for ECT a little while ago. Ended up doing a bit of research and the inevitable n=1 dose finding over the treatment course. Roc dose of 0.5mg/kg with reversal with 6mg/kg of sugammadex worked well. The issue is waiting a bit longer and therefore needing more propofol
 Raj LB (@rajlb.bsky.social) reposted reply parent
Raj LB (@rajlb.bsky.social) reposted reply parent
How much rocuronium do you give? Purely curiosity - don't even know if we do ECT on site here.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
You can use HFNO to prevent desats journals.lww.com/ectjournal/a...
 Hans Huitink (@airwaymxacademy.bsky.social) reposted
Hans Huitink (@airwaymxacademy.bsky.social) reposted
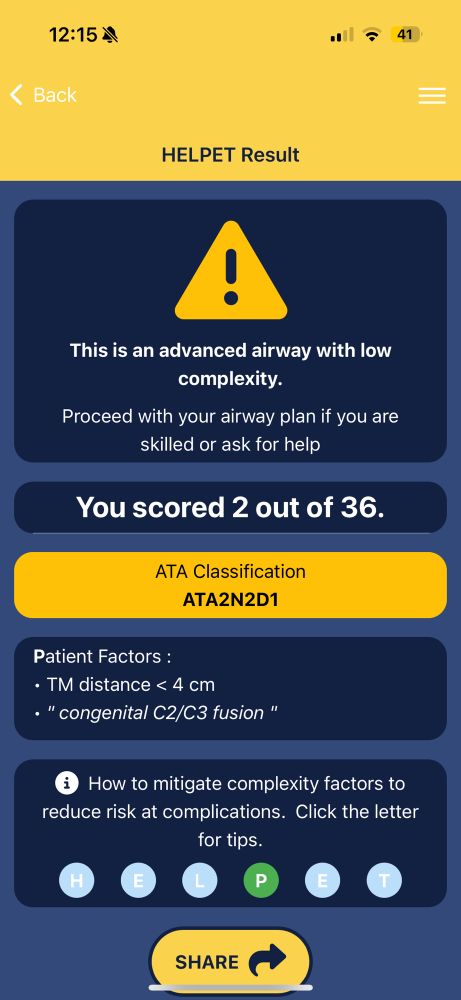
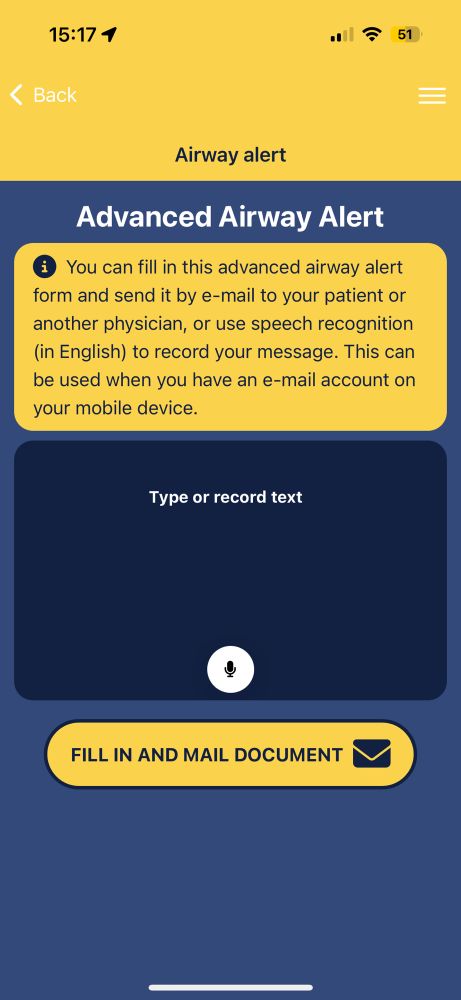
Do you need decision support for awake intubation? If “awake intubations alerts” pop-up on your airway triage app summary screen, discuss with the team if awake intubation is needed. @bobfunn.bsky.social @ncglasses.bsky.social @maffygirl.medsky.social @Hypoxicchicken.med-mastodon.com.ap.brid.gy
 Dr Michael Clifford (@drmikeclifford.bsky.social) reposted reply parent
Dr Michael Clifford (@drmikeclifford.bsky.social) reposted reply parent
VERY RARELY intubated - despite the drug addled fasting history (from the psych nurses - the patients rarely got it wrong), smoking, obesity, reflux etc. I am so old,I remember methohexitol - propofol is way better. I have seen non-sux ECT remifentanil, mivacurium and rocuronium. Sugammadex anyone ?
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Yes we use them. But why do you need a VL for ECT if you do not intubate… that was the question
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Do you intubate your patients for ECT???
 Hans Huitink (@airwaymxacademy.bsky.social)
Hans Huitink (@airwaymxacademy.bsky.social)
Do you need decision support for awake intubation? If “awake intubations alerts” pop-up on your airway triage app summary screen, discuss with the team if awake intubation is needed. @bobfunn.bsky.social @ncglasses.bsky.social @maffygirl.medsky.social @Hypoxicchicken.med-mastodon.com.ap.brid.gy
 Dr Mary-Ann Fox BMBS FANZCA GChPOM (@maffygirl.medsky.social) reposted
Dr Mary-Ann Fox BMBS FANZCA GChPOM (@maffygirl.medsky.social) reposted
Well that was quite a day on call. No one has ever appreciated a MAC 3 like me today. VL saved the day as I intubated on my knees. We do not always get the best operating conditions. We do not always intubate in theatre.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
What happened?
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
I generally go from 3 straight to D if I don't get it first go. During the initial COVID waves I started routinely using a bougie to improve my FPS rate, and it's just a short step from that to routinely using HAVL + stylet/steerable bougie from there. I teach VADL but use (HA)VL routinely.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
I almost never use a size Mac 4 blade when using VL. Mostly a 3. It makes tube delivery with VL a bit more difficult because the bulky blade needs space in the larynx
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Many departments of anaesthesia have insufficient numbers of VL. Even in the “rich countries”. They do not priorities it on yearly budgets and rather spend money on new ultrasound machines it seems…
 Vin Vyapury (@bluntingstress.bsky.social) reposted reply parent
Vin Vyapury (@bluntingstress.bsky.social) reposted reply parent
Having immersed in Vortex workshops in the last 12 months, I can see its value in a system where everyone understands it/and its terminology. However, when DAS algorithms are taught and executed right, it brings about the same outcome.
 Manu B (@nitrousman75.bsky.social) reposted reply parent
Manu B (@nitrousman75.bsky.social) reposted reply parent
Its is a cognitive aid & that’s what’s needed in an airway crises to avoid fixation errors . Don’t ever recollect anyone reading out a DAS algorithm in my 23 yrs in anesthesia during a dynamic , rapidly evolving situation such as an airway crises .
 Hans Huitink (@airwaymxacademy.bsky.social)
Hans Huitink (@airwaymxacademy.bsky.social)
🎥 vimeo.com/showcase/118... Short airway triage app tutorials Download the app from the app stores Google play.google.com/store/search... Apple 🍎 apps.apple.com/nl/app/airwa...
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
The effectiveness of grading scores is totally overrated. Every intubation is unique because the context is different. Different indication, different intubator, different physiology, different medication, different position, different device. A previous view at the larynx does not predict a lot.
 Stu Marshall (@hypoxicchicken.medsky.social) reposted
Stu Marshall (@hypoxicchicken.medsky.social) reposted
Still using Cormack-Lehane grading for VL? Why?! Out today a new @bjaeducation.bsky.social article by @naomi-gostelow.bsky.social Bhavesh Patel and me looking at grading systems for VL. #AnSky #MedSky kwnsfk27.r.eu-west-1.awstrack.me/L0/https:%2F...
 Royal College of Anaesthetists (@rcoanews.bsky.social) reposted
Royal College of Anaesthetists (@rcoanews.bsky.social) reposted
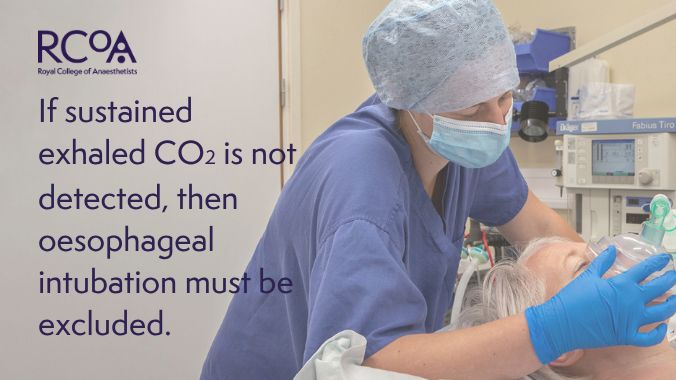
🚨We have retired "no trace, wrong place" to align with PUMA guidelines. Instead, with @assocanaes.bsky.social and @dasairway.bsky.social, our message is that if sustained exhaled CO2 is not detected, then oesophageal intubation must be ruled out. See our dedicated webpage👉 ow.ly/vOZs50WA03r
 Safe Airway Society (@safeairwaysociety.org) reposted
Safe Airway Society (@safeairwaysociety.org) reposted
The @universalairway.org guidelines for preventing unrecognised oesophageal intubation are supported by @safeairwaysociety.org, @anzca.bsky.social & @dasairway.bsky.social VL should be used routinely whenever feasible. Clinical signs should not be used to exclude oesophageal intubation.
 Raj LB (@rajlb.bsky.social) reposted reply parent
Raj LB (@rajlb.bsky.social) reposted reply parent
Ooh that's interesting. I used LMAs a lot when I first started. Don't know if they were they strictly 1st gen/classical (they were disposable for one) but required actually guiding into place. I do think the jump from a classical LMA to flexi is much smaller though.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Yes they are tricky, I use a stylet inside
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Forgive me, flexi LMAs are quite a bit trickier to site than classical 1st gen LMAs. They require an acquired knack that is different to the classic but you're right they're certainly different to iGels or the relatively more rigid 2nd gen Supremes and Ambu Auragains.
 Raj LB (@rajlb.bsky.social) reposted reply parent
Raj LB (@rajlb.bsky.social) reposted reply parent
My most recent bit of learning about teaching from this week is that trainees may be less familiar with siting flexi LMAs (because you basically site them like classical LMAs). The iGel has removed that skill. And I've only been a cons for a month!
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Different eras notwithstanding, I hope we can all agree, especially when it comes to complex airway management, that it is generally better to anticipate proactively than to be forced to react, however heroically.
 Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
When I trained we were not particularly taught to assess the airway but we were taught to manage an unexpected tricky airway..lots of mask holding, lots of ETTs , no SGAs..different eras need different understanding😊
 Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
Nice summary but even with preop airway assessment or not ..this would have gone better if the human factors had not been the main issue. Listen to those around you, give them a voice, stop trying to intubate when you are still able to ventilate etc 😔
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Fingers very helpful
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
She would not have been triaged as a basic airway: 1 shared airway with sinus problems 2 congenital C2/C3 fusion. 3 Maybe short TM distance or short neck? Add that to induction without preox and problems with flex lma, human factors and timepressure: recipy for disaster…
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
9/11 So- If this is something cataclysmic like this that could happen to me on any given day without my being able to predict it, I'm going to want those few but precious extra minutes during an airway crisis that preO2 provides so that I can gather myself, get oriented and aware, and do the drill.
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
8/11 And it need only happen once in a career for it to be catastrophic for everyone concerned: the patient most of all, but also the family, the anaesthetist, theatre team, everyone.
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
6/11 It's important because if it could happen to an experienced senior ENT anaesthetist that they assess an airway and deem it to be not complex or difficult, only to encounter an *unexpected* CICO on induction, it could happen to me.
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
5/11 The team then found themselves not just in a CICO situation, but in an *unexpected* CICO situation. This is an important detail.
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
4/11 ...this, on p7. Anaesthesia was induced at 0835, which means that in less than 2 minutes, her sats were already 75%. This suggests strongly that she had not been preoxygenated. Given her size and fitness had she had preO2 her sats should have stayed >90% for at least 3 min (and as much as 7).
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
3/11 This, on page 6. Now just because preO2 was not recorded, doesn't mean it wasn't given. However...
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
2/11 Elaine Bromiley was a lean otherwise fit 37yo ASA I mother of two,with no intercurrent medical problems other than a sinus condition (the indication for her operation). She was assessed preop by a senior anaesthetist who specialised in ENT cases, who did not anticipate any airway difficulties.
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
1/11 Let me analyse briefly how I've come to this personal recommendation. 🧵👇 First you need to read carefully Prof Michael Harmer's 2005 expert report into the case, made available to the public by the Bromiley family. emcrit.org/wp-content/u...
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Aw Jeez 🤦♂️ - if there's ONE thing we should all learn from the Bromiley case,*despite* Andy Lumb's work, it's that we should be routinely preoxygenating everyone unless there's an obvious contraindication (e.g. extreme mask phobia or demonstrated dependency on hypoxic drive)
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
I suspect patients are less interested in the process by which complications occur as they are by the consequences of those complications: "you could throw up/get a headache/suffer permanent brain damage/die" etc. Clinicians are more interested in process because then they know how to treat it.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Probably a mini-one for the mini patients?😇
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Never a dull moment Nick
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
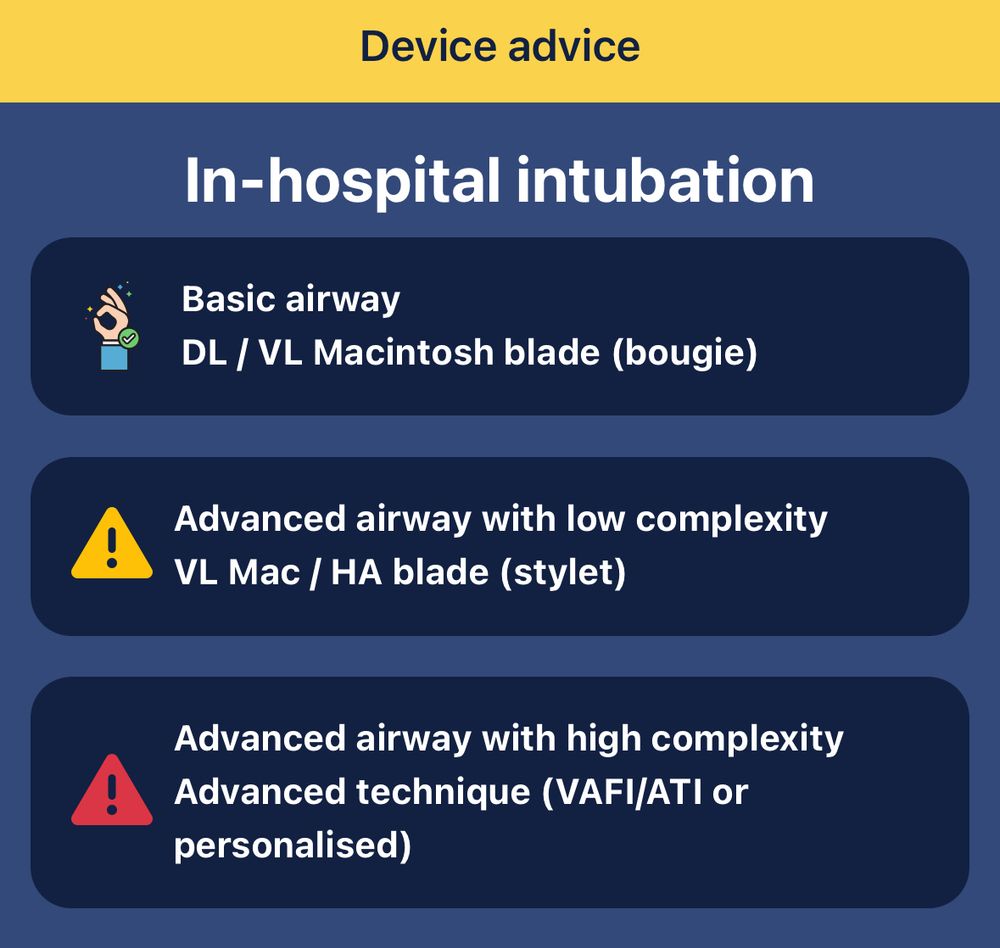
Better airway assessments methods will reduce the need for videolaryngoscopes. A VL really is not needed in patients who are classified as having a basic airway. Safety is paramount but can be reached much cheaper and faster. #airwaytriage
 Anaesthesia (@anaesjournal.bsky.social) reposted
Anaesthesia (@anaesjournal.bsky.social) reposted
There are economic and logistical factors which may limit the universal implementation of VL. BUT safety is paramount. Investment in this technology may be justified, particularly when considering the potential costs of failed tracheal intubation. #AnSky
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Use the PHASE or HELPET checklist to triage airways. Use a DL for basic airways, a VL for advanced airways. That works well. #airwaytriageapp #deviceadvice
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
So you sneaky sting us with a 🐝? I would not like that either…😂
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Good point but difficult to find out what is important 4all professions. I once started interscalene in combination with GA for upperarm ##. When I put US probe on neck I asked what profession pt had and then saw a giant bloodvessel… he said I am a lawyer and judge.. a code blue elsewhere saved me
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
6/15 [It's always good to get to know your patient. There was once an anaesthetist who offered a supraclavicular block to a patient, accepting (in their mind) the 0.3% risk of pneumothorax. They didn't ask the patient's job. The pt got a ptx - but he was a navy diver. He was unable to work again.]
 TomH (@thomhall.bsky.social) reposted
TomH (@thomhall.bsky.social) reposted
A good study on actual trained anaesthetists in Europe… we all know VL is good, so where is the guidance I can wave at purchasing to let us have more than one glidescope between seven theatres*? Said guidance also needs to let us train and maintain DL as a core competency (*hyperbole)
 Chris Nickson (@precordialthump.bsky.social) reposted
Chris Nickson (@precordialthump.bsky.social) reposted
Airway assistant (ala airway ally) litfl.com/airway-assis... the forgotten role in airway management in ED, ICU, and the wards… but an important one! #foamed #foamcc
 Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
Robbie Erskine (@drrobbieerskine.bsky.social) reposted reply parent
I agree with you both NAP3 is the only big series looking at neuraxial complications Significant Spinal haematoma associated with spinal anaesthesia was absent Whereas it demonstrated the patients we need to consider/monitor most carefully are the sick elderly patients with TEAs withmajor surgery
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
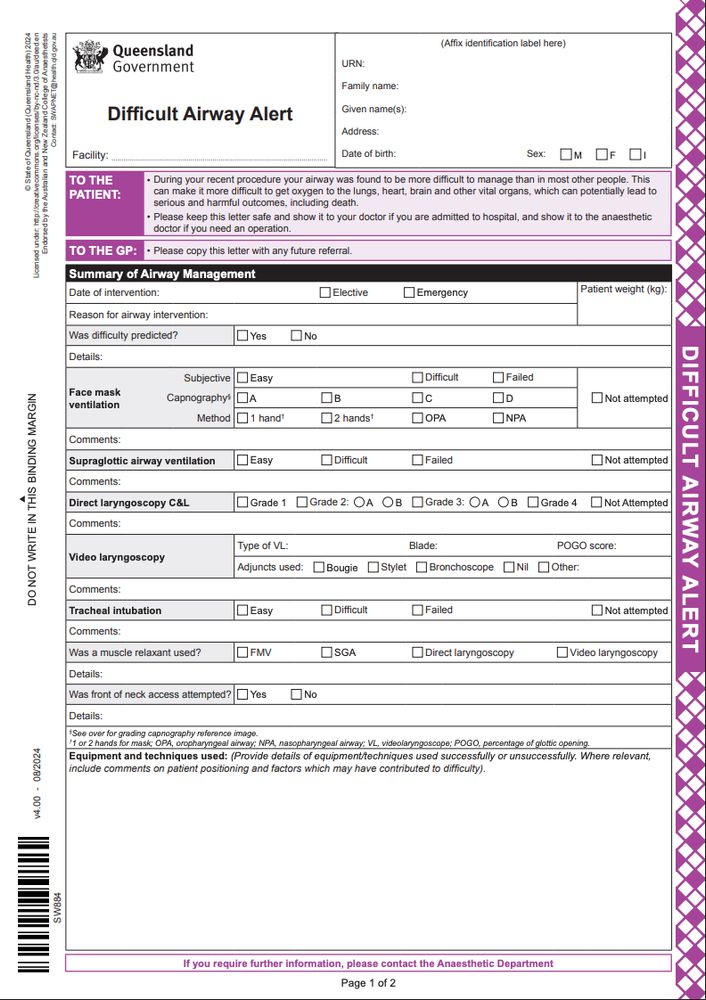
I use the advanced airway alert feature of airway triage app. It looks similar and can be mailed or shared with patient and caregivers. #airwaytriage
 Anaesthesia (@anaesjournal.bsky.social) reposted
Anaesthesia (@anaesjournal.bsky.social) reposted
What does your difficult airway alert form look like? Here's a standardised communication tool from Queensland. Thoughts? Similarities/differences from your institution? #AnSky #AirwaySky doi.org/10.1111/anae...
 Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
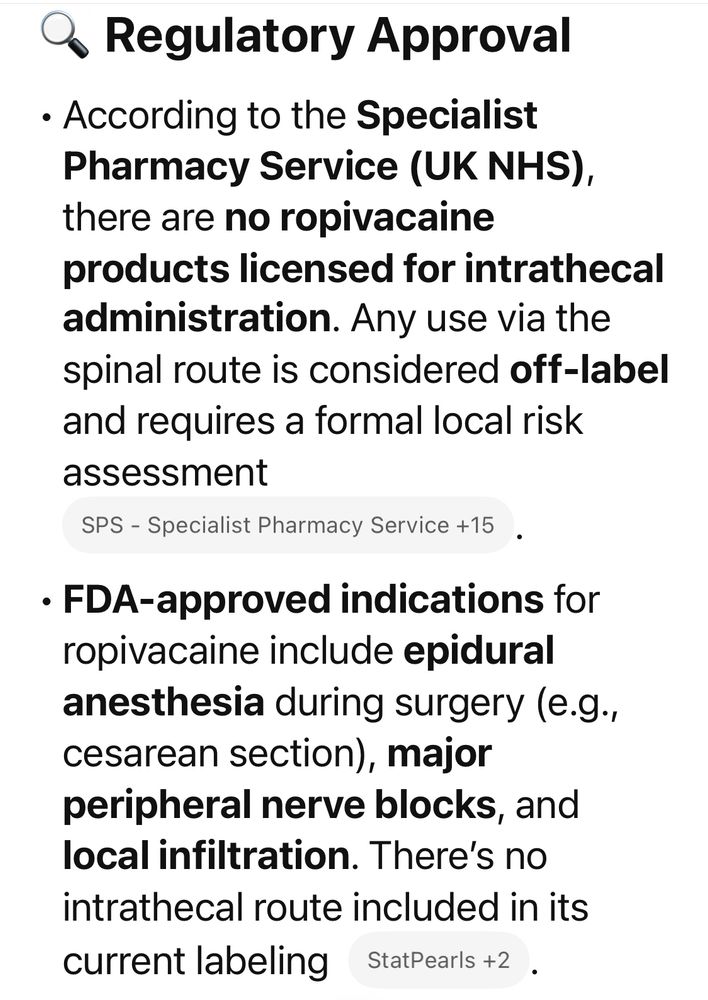
sounds excellent! unfortunately Ropi intrathecal here is a no. Also we don’t have dilute morphine (ours is 5mg/ml) so potential big error.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Not for intrathecal use
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
During my training we uses bupivacaine 0.5% plain for csections with similar effect
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
I've been doing ropi/fent spinals for caesars for about 20 years. Main advantages are that it's extremely fast and if you get significant hypotension you can tip the pt into trendellenberg without making things worse. Our local audit showed it also causes less urinary retention.
 Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
chatGPT says:
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Are you using ropi for spinals? Is that off label use?
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
On dental lists I use a freezing spray (we don't have ethyl chloride in Oz anymore) to stiffen the curve of the tube into the shape I want (like putting the old red rubber tubes in the Quality Street tin for blind nasals). Makes instrument free intubation somewhat easier.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Airway hero level “Mythic” if you had used airway triage app for all those patients
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Agree with you Bob
 Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
very oddly imo - this clopidogrel angst ultimately comes from guidelines that have been printed with indelible ink that make no differentiation between tiny thin spinal needles that just go in and out and thick tuohys through which a catheter is shoved in. All just called neuraxial block.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
If you can explain to family and patients that in your opinion spinal would be better or “safer” and you tell them the very low incidence of spinal hematoma I think it is acceptable risk to use spinal technique. Most of our old and frail NOF pts will have spinals. Occasionally general anaesthesia
 Hans Huitink (@airwaymxacademy.bsky.social)
Hans Huitink (@airwaymxacademy.bsky.social)
24/7 airway teaching with Mobile Airwaycase Generator (MAG) of @AirwayTriageApp More then 10000 advanced airway cases. Make the case, discuss a strategy and do the sim. This is how it works 🎥 #airwayteaching #airwaytriage #meded #anaesthesia #criticalcare #MAG
 Hans Huitink (@airwaymxacademy.bsky.social) reposted
Hans Huitink (@airwaymxacademy.bsky.social) reposted
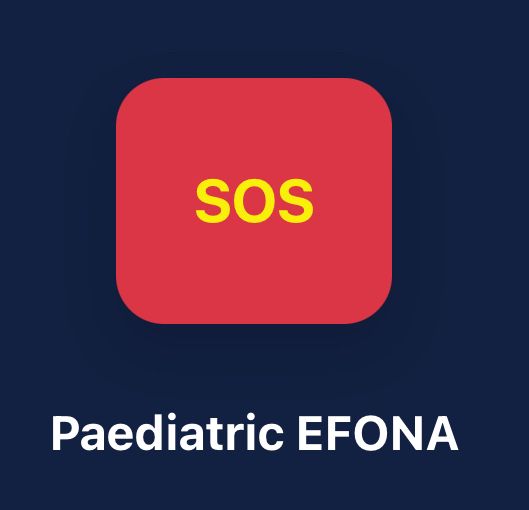
Airway Triage App update 6.5.32 is available now. Great new features. 📌paediatric EFONA 📌post intubation checklist 📌my intubations Available on the app stores #airwaytriageapp
 Hans Huitink (@airwaymxacademy.bsky.social)
Hans Huitink (@airwaymxacademy.bsky.social)
Update your Airway Triage App for free
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Google play store play.google.com/store/apps/d...
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
🍎 apps.apple.com/nl/app/airwa...
 Dr Pieter Peach (@pieterpeach.com) reposted reply parent
Dr Pieter Peach (@pieterpeach.com) reposted reply parent
Would be great have a link to a website with all the App Store download links
 Hans Huitink (@airwaymxacademy.bsky.social)
Hans Huitink (@airwaymxacademy.bsky.social)
Airway Triage App update 6.5.32 is available now. Great new features. 📌paediatric EFONA 📌post intubation checklist 📌my intubations Available on the app stores #airwaytriageapp
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Yes it can be a reliable predictor but if the patient needs to be intubated in bed it will be totally different than in the ct scanner. Even with best positioning. The context will never b the same. If they intubate <3 minutes, the cords may still be partially closed…too many variables.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Interestingly we could stop documenting our best view as every airway management procedure is unique in itself and the context will never b the same. Predictive power of a good/bad glottic view for a next intubation is low as next procedure will b different (procedure, airway manager, physiology)
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
So pogo is the easiest. 100-75-50-25-10-0 The subclasses are too complex in my opinion
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Grade 1 view 😳
 Sam Goodhand (@samgoodhand.bsky.social) reposted
Sam Goodhand (@samgoodhand.bsky.social) reposted
I need your help! The airway checklist card initiative grew to 17,000 cards across the 🌍, supported by major bodies & heavily propelled by Twitter 🪦. Please help me re-spread the message with a repost! Adult, paediatric & global (LMIC) versions. NFP. checklistcard@outlook.com. #patientsafety
 Sam Goodhand (@samgoodhand.bsky.social) reposted
Sam Goodhand (@samgoodhand.bsky.social) reposted
Wise words from Capt Neil Jeffers at #GAMC2025 - we’re obsessed with leadership in medical emergencies and don’t focus enough on followership.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Yes I like it 😎
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Then you have not intubated really advanced highly complex airways? Always first pass attempt? Always 100% POGO?🫣
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
CMAC Slim line has arrived now
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
14093 lol. Wanneer gaan we eten?
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
I cannot leave 14K followers just because 1 person is behaving weird. I have a message to tell and the interaction is still much better on X than on Blue
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Oh yes
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Yes i am very delighted
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
What Bob said 👆 plus 1) Sorta depends on why you're doing an inhalational: needle phobic/complex airway/just for kicks 2) 'Single breath induction' (in reality 'Several Breath Induction') is useful in cooperative adults 3) Entonox+sevo also useful but not for complex airways where you need 100% O2.
 Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Now start O2 & volatile. Get them to breath with mouth open - this is important. It helps reduce the smell of volatile. Also prevents them talking 😉 Be firm with the mask. Explain what you want, tell them they’re doing great.
 Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
Bob Funnekotter (@bobfunn.bsky.social) reposted reply parent
First: make sure OR environ is “sleep conducive”: dim the lights, no noise or distractions. Keep everything as boring as possible. Only the necessary peeps present. Do all the checklists and attach all the monitors.
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Agree
 Ross Kennedy (@rrk310.bsky.social) reposted reply parent
Ross Kennedy (@rrk310.bsky.social) reposted reply parent
Late to this discussion but putting my hand up as someone who has occasionally put tubes & LMAs in before iv access. And would do so again if needed. Usual scenario is inhal induction then an assistant who is unable to place iv & for reasons I don’t want to hand over the airway to them*
 Hans Huitink (@airwaymxacademy.bsky.social) reply parent
Hans Huitink (@airwaymxacademy.bsky.social) reply parent
We do a lot of volatile inductions in the dental office in patients who are too young or too anxious for iv induction. Normally this is smooth if you make sure the arms and hands are fixated by a helper when you put in the iv as this may cause a muscle contraction reaction
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
You think you're looking at things through an 'objective' lens, but in fact you are looking at things through an 'young' lens. Some things you consider 'safe' now will be deemed an atrocity 20 years from now. 'Objectivity' is a product of consciousness which is by definition a subjective experience
 Manu B (@nitrousman75.bsky.social) reposted reply parent
Manu B (@nitrousman75.bsky.social) reposted reply parent
Don’t have Glidescope at the hospitals I work at . Why I like McGrath over CMach is cos it’s smaller , lighter , slimmer blade (sleek ?) compared to CMach . I also like the screen on the handle. I do a lot of spines (older patients) in private hospitals & this seems ideal .
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
I use them all the time and I have no complaints technically. VL is now my routine. But as a teacher I think trainees should learn both VL and DL techniques, so I prefer a device that can do both. Nothing is more dangerous than a plan/device/technique when it's the only one you have.
 Dr Mary-Ann Fox BMBS FANZCA GChPOM (@maffygirl.medsky.social) reposted reply parent
Dr Mary-Ann Fox BMBS FANZCA GChPOM (@maffygirl.medsky.social) reposted reply parent
I think you need to assess your environment and I am privileged to have access to a multitude of devices. I like the big screen because your assistant can see how their airway maneuvers can change with them changing techniques. Love educating the room as well. Gets them off their phones!!!
 Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
Nose Coloured Glasses (@ncglasses.bsky.social) reposted reply parent
I agree @maffygirl.medsky.social. Beyond a certain point asking whether one particular VL is better than other is a bit like asking if a steak knife is better than a fish knife. Depends what you're using it for.
Stu Marshall (@hypoxicchicken.medsky.social) reposted reply parent